(Des Moines) Iowans stressed the importance of health coverage and the difficulties of obtaining government recognition of medical conditions at the first public comment session on state’s effort to add work requirements to its expanded Medicaid program.
The Iowa Department of Health and Human Services is seeking a waiver from the federal government allow it to implement work requirements for the Iowa Health and Wellness Plan, or IHAWP. The public hearing Wednesday at the Urbandale Public Library was the first of three meetings for public comment required by the waiver submitted to the U.S. Centers for Medicare & Medicaid Services.
IHAWP is the Medicaid expansion program signed into law by former Gov. Terry Branstad, a Republican. It provides public health insurance for low-income Iowans at or below 133% of the federal poverty level who do not qualify for regular Medicaid coverage — people between the ages of 19 to 64 who do not have a disability.
The waiver, announced by Gov. Kim Reynolds earlier in April, proposes requiring IHAWP recipients to work 100 hours per month to remain eligible for coverage. There are other ways to meet this requirement — a person can continue receiving state health coverage if they are enrolled in an education or job skills program, or if they earn the equivalent in wages to working 100 hours a month at the state minimum wage, $7.25 per hour.
There are some exceptions for the work requirements. People who are considered medically frail or medically exempt under Medicaid would not have to meet the work requirements, nor would individuals caring for a child under age 6, who have a high-risk pregnancy, or are in substance abuse treatment programs for up to six months. The waiver request also states that individuals who “provide proof of good cause as defined by HHS” would be exempt, but did not include details on what standards would be used by the state department for assessing these claims.
At the hearing, several speakers talked about their own experiences or time helping others applying for public assistance coverage under the current Medicaid program. Nancy Lynch of Des Moines, a former school social worker, said she worked with parents of children with disabilities who were denied services and assistance — and said she believes work requirements would add another hurdle for people in need accessing health coverage and care.
“My job was to help support parents who had children with very special needs that needed help — needed help with health care, needed help with services — and I saw how difficult it was for them to receive those services,” Lynch said. “No one got it on the first time. Everybody had to apply three and four times. They’d say the same thing, but they had to reapply and reapply and reapply. So they had to kind of beat down the system until they were finally accepted. … And my big concern is that these work requirements will add more barriers to people who need these services, they will lose the support they need.”
Robbin Mensching of West Des Moines said she was concerned about how HHS would assess mental illnesses and provide exemptions. Speaking about her own experience struggling to receive an official diagnosis of having a mental illness, she said it can be difficult for people with mental health issues to be recognized as having a medical issue. After receiving care, Mensching said she was able to more fully participate in life, but that denying that coverage could impact people’s ability to join the workforce or care for their families.
“I want to know how they’re going to handle covering these people, because there are a lot of people that have been like me,” Mensching said “Anxiety, depression, panic attacks — it’s disabling.”
Work requirements would be enforced through reporting. HHS stated that people on IHAWP would be required to report information showing the work requirements were met every six months. The department plans to create a mobile application for IHAWP members to submit required information showing their compliance with the work requirements if HHS does not already have the information available. If the required information is not provided, the individual’s coverage would be suspended.
Mary Nelle Trefz, the advocacy network director of Iowa ACES 360, called for the state to share information about the cost of implementing work requirements, pointing to the need for the Iowa state government to create a new information technology system and train staff to implement and support the reporting requirements.
As Reynolds and HHS pursue a waiver for implementing work requirements, the Iowa Legislature has also moved this session to pass a bill implementing expanded Medicaid work requirements. There are some differences between the HHS and legislative policies — the bill proposes an 80-hour monthly work requirement, and includes “trigger” language that would require the state to end IHAWP coverage for all recipients if the federal government revokes work requirements in the future after they were approved.
The legislation also includes an appropriation of roughly $8.2 million, according to the Legislative Services Agency, to set up the needed IT system for administering reporting requirements under the proposal. The funding to create this IT system is not a part of the HHS waiver request, Trefz said.
“That pending legislation also included support for IT, funding for that — but that legislation has not passed yet,” Trefz said. “Those dollars have not been appropriated. So how will the state ensure the necessary infrastructure is in place?”
Multiple speakers expressed frustration that the HHS staff who hosted the meeting did not answer several of the questions or direct responses from HHS or other state leadership posed about certain details of the policy or how it would be implemented, or if there would be changes made to address any of their concerns. Staff at the meeting said the comments and questions would be shared with state leaders, and would be used to answer questions about work requirements in future communications.
Mensching said she felt work requirements were already a “done deal” in Iowa, but said she believed it was important for Iowans — especially those who would be impacted by the change — to speak out.
“I would have ended up living on the street at one point in my life (without health coverage), and then you’ve got all these other things that go with that — somebody getting health care for me, the police would be involved — I mean, it just goes on and on,” Mensching said. “It’s so much more efficient and humane to just give people coverage so that they can live a normal life.”
Trefz, alongside Stacy Frelund with the American Heart Association, said they were creating a “protect Medicaid” coalition to coordinate organizing efforts to oppose the new work requirements.
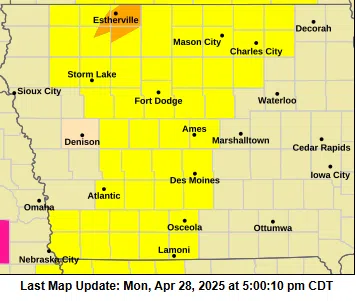
There will be another public hearing held on the waiver request, on April 29 at 2 p.m. at Marshalltown Public Library. Comments can also be submitted through email and by mail through May 15, with information available on the public notice website for the waiver.
From left: Terry Anderson, Heather Sanders and Robbin Mensching raised their hands to make comments or ask questions of Iowa Department of Health and Human Services staff about the state’s proposal to add work requirements to the state’s expanded Medicaid program, Iowa Health and Wellness Plan, during a public comment session hosted at the Urbandale Public Library April 23, 2025. (Photo by Robin Opsahl/Iowa Capital Dispatch)